Liver Disease Treatment
Working Together Making a Difference
LIVER DISEASE TREATMENT: WHAT & HOW?
Comprehensive Liver Disease Treatment & Education In Tucson, Arizona



How The Liver Institute Cares For Liver Disease Patients
Diagnosis
If you suspect or notice summon signs of liver disease, The Liver Institute specialists can help identify and diagnose possible liver damage. While it’s common to think alcohol is the primary cause, early stages of liver disease can manifest due to viruses or bacteria.
Treatment & Reversing Damage
Liver disease treatment begins as soon as possible after diagnosis. The idea is to take a multi-faceted approach to healing the liver and reversing any existing damage. The Liver Institute is proud to use a variety of tests and imaging to create a recovery plan.
Monitoring & Management
For patients with chronic liver disease, or reoccurring liver damage, we create individualized action plans for life-long management. We give you the tools you need to monitor your progress and prevent future damage.

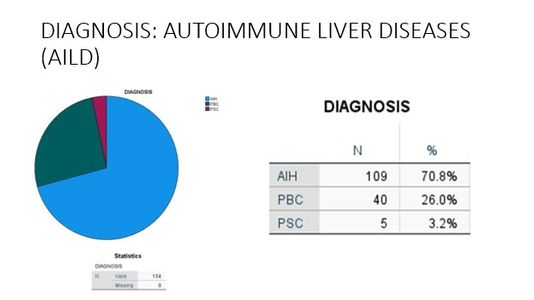
Diagnosing & Staging Of Primary Liver Disease
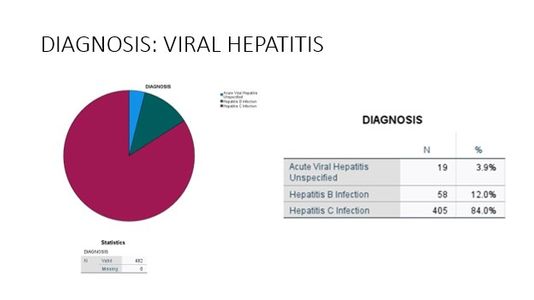
Like any other organ, the liver can be injured or damaged due to several reasons. Generally, it is perceived that alcohol is the only cause of liver damage leading to cirrhosis. However, with the liver being the organ to process and metabolize all the ingested nutrients, chemicals, or toxins, there is potential to have damage due to inadequate functions of nutrients and chemicals/medications and metabolic dysfunction. Moreover, exposure to viruses, bacteria, or other pathogens, and surgical or accidental trauma, can result in serious acute or chronic liver damage. Several patients may have more than one factor causing liver damage. Our comprehensive approach at the Liver Institute is to identify all the possible factors involved in the causation of liver disease and assess the degree of damage at the baseline. We provide liver disease treatment for all possible factors and monitor the response to assure healing or get ready for alternative life saving options, such as liver transplantation.
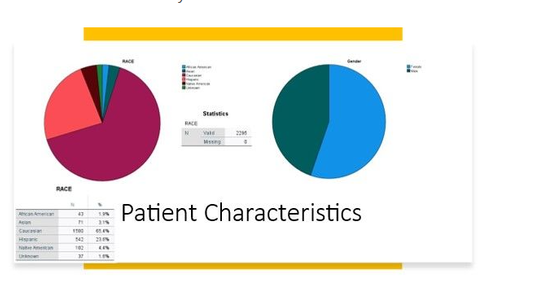
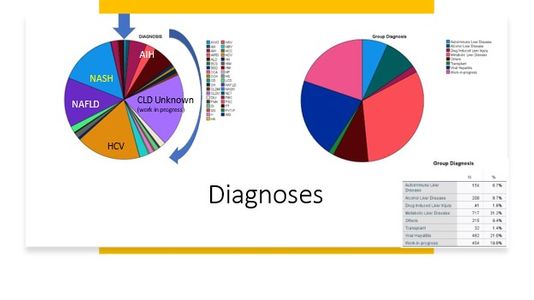
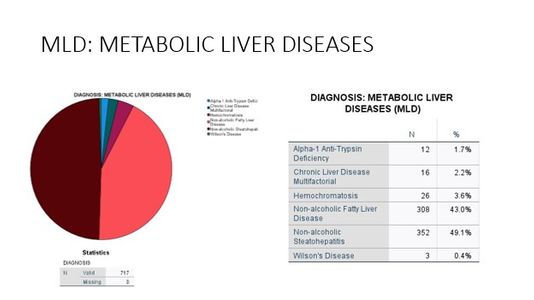
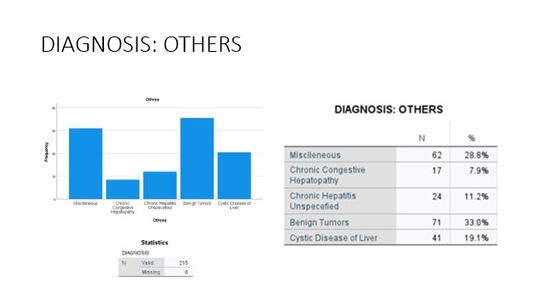
Liver Disease Distribution
At The Liver Institute, we see a variety of liver diseases in patients across Arizona. No matter what unique situation you may be dealing with, our liver disease treatment and management is unlike any other. If you believe any of the following situations apply to you, contact us right way!
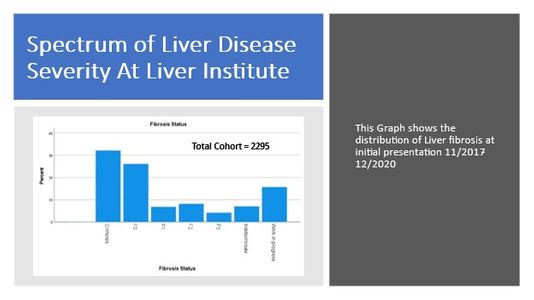

Treating Liver Disease To Reverse The Damage
It was generally known and understood that once advanced liver damage such as cirrhosis happens, it does not recover. But new research in the past few years has provided sufficient scientific evidence to change our concepts and understanding of liver disease treatment and monitoring. By eliminating all the possible hepatotoxic factors, healing of the liver is expected even at the cirrhosis stage, though it is time-driven. A liver biopsy is needed to demonstrate the recovery and healing after a period of treatment. Non-invasive tests could be used as a surrogate marker to monitor the healing process. At The Liver Institute, we use a combination of clinical imaging (ultra sonogram and Elastography), and blood tests parameters to assess the recovery process.
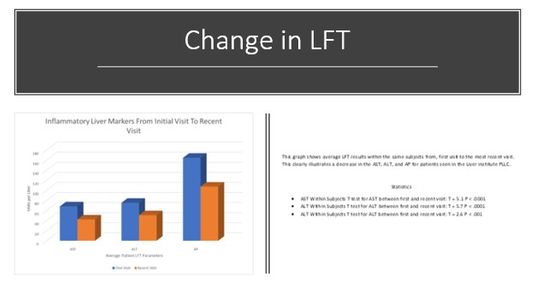
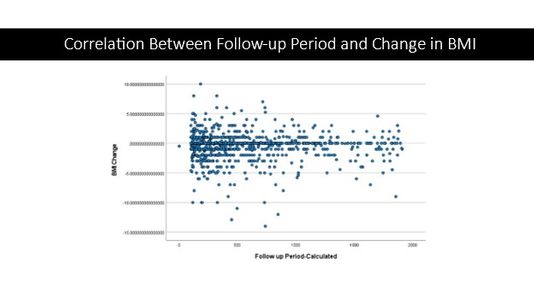
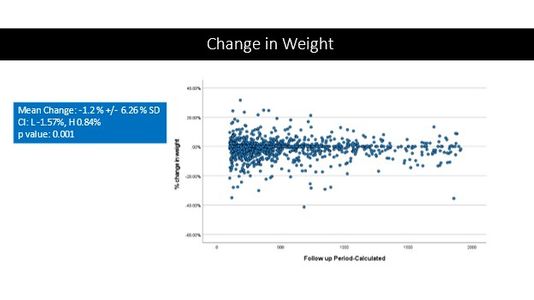
Trends In Liver Function Tests (LFT)
New data in the diagnosis and treatment of liver disease shows a change in how the liver’s functions correlate to a patient’s weight and BMI. The Liver Institute provides a comprehensive liver disease treatment plan that includes analyzing and improving a patient's nutrition and diet.

Management of Cirrhosis
Cirrhosis, a final pathway for a wide variety of chronic liver diseases such as fatty liver disease/NASH, viral hepatitis B or C, hereditary diseases etc. Cirrhosis is an advanced stage of liver damage. Appropriate identification of this milestone is crucial as it reflects the risk of emergence of life-threatening complications.
Cirrhosis may be classified broadly as compensated (without life threatening complications) or decompensated (with life threatening complications). The development of complications such as variceal hemorrhage, ascites, encephalopathy, jaundice, or hepatocellular carcinoma characterizes decompensated cirrhosis. In compensated cirrhosis, these complications are absent.
Our liver disease treatment approach to management of cirrhosis is multifaceted. This includes emphasis on identification and treatment of primary liver disease as described above (precise diagnosis and stage of primary liver disease), which will help achieve regression (down staging) or prevent progression of fibrosis stage in a good proportion of patients. This is especially effective when it is at the compensated phase. The second goal is to prevent life-threatening complications such as portal hypertension, liver failure and liver cancers. Reduction in the risk of life-threatening complications is the principle of management, which is achieved by:
Consistent adherence to screening, surveillance, and treatment of superimposed drug
Herbal or supplements induced liver damage
Infections involving liver or other organs
Concurrent medical conditions affecting liver
Lifestyle intervention management
Cessation of alcohol
Appropriate surgical risk assessment and management, prior to any procedure or surgical intervention, is needed to reduce the risk of complications and death post procedure.

Management of Portal Hypertension
The portal venous system carries blood enriched with nutrients and ingested chemicals such as medicines or herbs from the esophagus, stomach, small and large intestine, pancreas, gallbladder, and spleen to the liver. In advanced liver fibrosis, blood flow through the liver is impaired due to destruction of small blood vessels as a result of fibrosis or scarring. This results in increased portal blood flow resistance, which is called portal hypertension.
Portal hypertension almost always results from increases in both portal resistance and portal flow. Emergence of such high-pressure liver circulation increases the risks of life-threatening complications such as sudden onset variceal hemorrhage, chronic bleeding from stomach and colon, accumulation of fluid in abdomen (ascites), kidney damage, infections in the ascites fluid and other cardio-pulmonary complications.
Management of portal hypertension is complex, and the ultimate treatment is a liver transplantation, which is an option in only a minority of patients. Others depend highly upon skilled management to prevent treatment of life-threatening gastrointestinal bleeding, ascites, control of pulmonary hypertension, screening, surveillance, and preservation of kidney functions, and screening and treatment of intrapulmonary shunts. Treatment and management include very diligent and judicious use of:
Diuretics
Non-selective beta blockers
Diagnostic and therapeutic paracentesis (often recurrent)
Antibiotic prophylaxis
Endoscopic screening
Surveillance and treatment of varicose veins
Gastropathy and gastric antral vascular ectasia (GAVE)
Identification and treatment of iron deficiency anemia
ECHO of heart
Right heart catheterization
Close monitoring of kidney functions with blood tests
Avoidance of use of drugs or toxins that may cause harm to kidneys
Finally, trans-jugular intrahepatic portosystemic shunt (TIPS) is an option in a highly selected group of patients, as creation of such shunt in the liver is not without risk of complications or death. A thorough pre-TIPS evaluation, planning and post TIPS management is needed to have successful outcome, control of portal hypertension with resolution of ascites and risk of gastrointestinal bleeding.

Management of Chronic Liver Failure
Chronic liver disease and liver failure disrupt normal homeostasis and cause systemic manifestations that may dominate the clinical features of liver disease. Manifestations of chronic liver failure include:
- Fatigue
- Decrease in sexual desire and functions
- Jaundice
- Easy bruising and thinning of skin
- Prolonged bleeding from cuts, nose and gum bleeding
- Loss of appetite
- Muscle wasting (sarcopenia; loss of muscle mass)
- Encephalopathy (difficulty maintaining focus and concentration, cognitive impairment)
- Deterioration of functional ability and self-care
Severity of chronic liver failure is assessed with combination of multiple tools such as MELD-Na score, Child- Turcotte-Pugh (CPT) score, White Haven Criteria, Encephalopathy App, smartphone-based Stroop test, and muscle mass assessment.
Most of these manifestations are reversible with liver transplantation, which is an option in only a minority of patients. Others depend highly upon skilled management to control such manifestations and preserve functional ability. Key management includes assessment and treatment of nutrition and lifestyle in conjunction with medication. Avoidance of polypharmacy is of paramount importance. Other factors include assessment and treatment of hormonal functions such as thyroid, adrenal, or sex hormones. Consistent adherence to screening, surveillance and treatment of osteoporosis and related complications of bone fractures help maintain functional ability.
